Blood transfusions
When hemoglobin exhibits particularly low values, typically below 8g / dL, the physician may decide to proceed with red blood cell transfusions, but sometimes platelet transfusions are also required. This will increase the blood values, with an improvement of the symptoms. In the case of red blood cell transfusions prolonged for months, it will also be necessary to remove excess iron with therapies called iron chelators.
Iron Chelator therapy
This therapy is used when the patient has “iron overload”, so it is aimed to eliminate the excess of iron that accumulates as a result of red blood cell transfusions and which can cause problems to vital organs (heart, liver, endocrine glands ).
Growth factors – Red blood cells stimulating agents
It consist in the administration of the artificial version of hormones already present in the blood, stimulating it to produce more red blood cells and white blood cells.
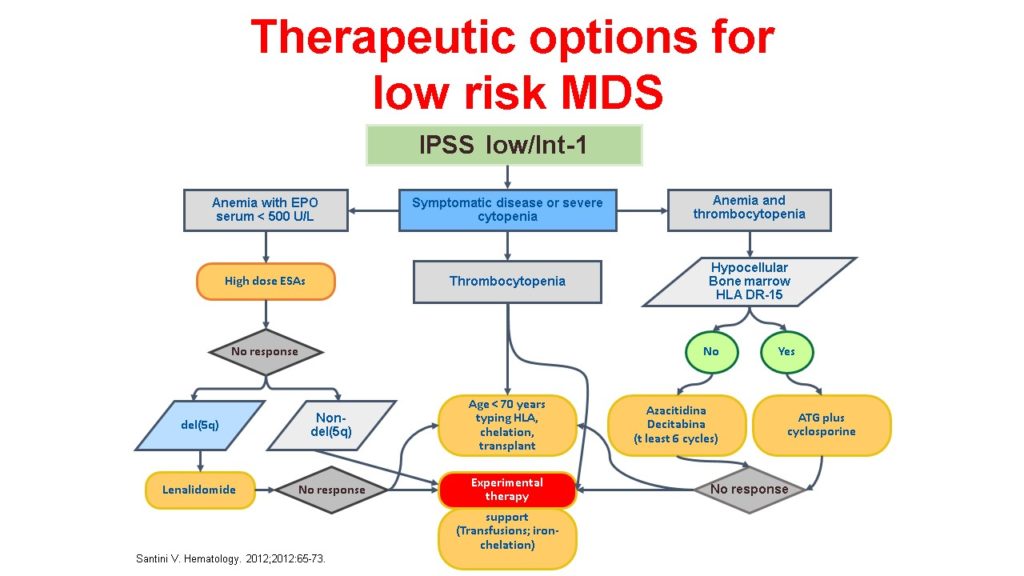
Some growth factors, such as erythropoietin (EPO) or Darbopoetin alpha, may affect the production of red blood cells and decrease or eliminate the need for blood transfusion. In some anemic patients, in fact, their EPO level is not sufficient to stimulate the sick bone marrow and in these cases the administration (subcutaneously) of synthetic erythropoietin (produced in laboratory) can be anf help. This therapy is effective in the majority of patients and it is chronic.
Other growth factors, on the other hand, are given to stimulate white blood cells, helping to treat the recurrent infections due to neutropenia, but they are not administered continuously.
Lenalidomide
It is an oral drug specifically used in myelodysplasia with deletion of chromosome 5q and requiring blood transfusions. Lenalidomide interferes with the immune system activity by blocking cell growth with chromosomal abnormality. In these cases it has a very high efficacy, sometimes reaching to normalization of hemoglobin levels.
Immunosuppressive Therapy
It is especially indicated in low-risk myelodysplastic syndromes, in patients not too elderly and in good general conditions, which have a non-populated bone marrow and some clinical and biological characteristics. This therapy decreases the immune response with the aim of preventing the destruction of bone marrow’s hematopoietic cells and allowing the stem cells to grow, resulting in improved blood values.
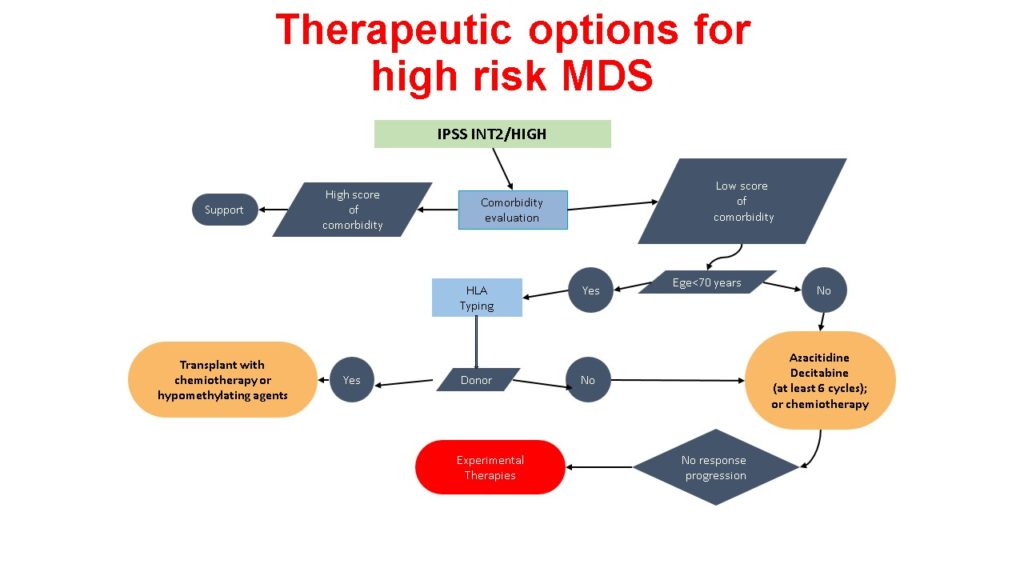
Hypomethylating drugs
In patients with intermediate-high IPSS risk not eligible for transplant or high-dose chemotherapy, may be used this type of therapy (5 Azacitidine and Decitabine), which, by lowering DNA methylation levels, reprogram the myelodysplastic cells and renovate their function and production of healthy cells. Azacitidine is given as outpatient treatment and is the only one of the two hypomethylating agents approved in Europe for the treatment of myelodysplasia, while Decitabine is approved only for elderly acute myeloid leukemia.
Chemotherapy
In cases of high or intermediate 2 IPSS risk myelodysplasia, there is a greater probability of having an acute myeloid leukemia evolution. Sometimes the physician can opt for intensive chemotherapy with the aim of killing abnormal bone marrow cells. This type of therapy is normally used in young patients and / or who can be transplanted (and who have no other serious associated illness). It is a therapy that requires hospitalization in isolation for a long time and should always be followed whenever possible by transplant.
Stem cell transplant
It is also sometimes called bone marrow transplant. The procedure first involves the administration of a preparatory chemotherapy that destroys all bone marrow cells and then the reinfusion in the patient of healthy donor stem cells, which have the task of repopulating the blood and the marrow itself.
However, this procedure is not always applicable due to the lack of a suitable donor, or the presence of comorbidities or other risk factors (such as older age that makes more fragile) that make it difficult or completely exclude the choice of this therapeutic approach.